Abstract
BACKGROUND
In the primary analysis of the Aspirin in Reducing Events in the Elderly (ASPREE) trial, now published in the Journal, we report that the daily use of aspirin did not provide a benefit with regard to the primary end point of disability-free survival among older adults. A numerically higher rate of the secondary end point of death from any cause was observed with aspirin than with placebo.
METHODS
From 2010 through 2014, we enrolled community-dwelling persons in Australia and the United States who were 70 years of age or older (or ≥65 years of age among blacks and Hispanics in the United States) and did not have cardiovascular disease, dementia, or disability. Participants were randomly assigned to receive 100 mg of enteric-coated aspirin or placebo. Deaths were classified according to the underlying cause by adjudicators who were unaware of trial-group assignments. Hazard ratios were calculated to compare mortality between the aspirin group and the placebo group, and post hoc exploratory analyses of specific causes of death were performed.
RESULTS
Of the 19,114 persons who were enrolled, 9525 were assigned to receive aspirin and 9589 to receive placebo. A total of 1052 deaths occurred during a median of 4.7 years of follow-up. The risk of death from any cause was 12.7 events per 1000 person-years in the aspirin group and 11.1 events per 1000 person-years in the placebo group (hazard ratio, 1.14; 95% confidence interval [CI], 1.01 to 1.29). Cancer was the major contributor to the higher mortality in the aspirin group, accounting for 1.6 excess deaths per 1000 person-years. Cancer-related death occurred in 3.1% of the participants in the aspirin group and in 2.3% of those in the placebo group (hazard ratio, 1.31; 95% CI, 1.10 to 1.56).
CONCLUSIONS
Higher all-cause mortality was observed among apparently healthy older adults who received daily aspirin than among those who received placebo and was attributed primarily to cancer-related death. In the context of previous studies, this result was unexpected and should be interpreted with caution. (Funded by the National Institute on Aging and others; ASPREE ClinicalTrials.gov number, NCT01038583.)
The Aspirin in Reducing Events in the Elderly (ASPREE) trial was a primary prevention trial that was established to investigate whether the daily use of 100 mg of enteric-coated aspirin would prolong the healthy life span of older adults.1,2 The trial, which was conducted in Australia and the United States, recruited 19,114 relatively healthy older persons from community settings. The primary end point was disability-free survival, which was defined as survival free from dementia or persistent physical disability. The primary composite end point was derived from the first end-point events of death, dementia, and persistent physical disability. The use of low-dose aspirin did not differ significantly from placebo in influencing the rate of the primary end point after a median of 4.7 years of follow-up.
When we took into account all occurrences of death, dementia, or persistent physical disability (regardless of whether they contributed to the primary composite end point), the incidence of each individual component did not differ significantly between the two trial groups. Overall mortality was higher in the aspirin group than in the placebo group, but not to an extent that reached significance if the P value was corrected for multiple comparisons. Other primary prevention trials of aspirin have not identified similar higher all-cause mortality.3-12 In this article, we examine the higher mortality in the aspirin group of the ASPREE trial, focusing on specific causes of death.
METHODS
TRIAL DESIGN
The trial involved men and women from Australia and the United States who were 70 years of age or older (or ≥65 years of age among blacks and Hispanics in the United States) (Tables S1 and S2 in the Supplementary Appendix, available with the full text of this article at NEJM.org). Details regarding the trial methods have been published previously,13 and the protocol is available at NEJM.org. In brief, participants were randomly assigned to receive 100 mg of enteric-coated aspirin daily or matching placebo. In Australia, recruitment involved collaboration with the participant’s usual primary care physician. In the United States, recruitment was community-based through academic health centers. The trial intervention was stopped on June 12, 2017, at the request of the funding agency, the National Institute on Aging, because results of conditional power analyses indicated that it was extremely unlikely that continuation of the trial intervention would reveal a benefit with regard to the primary end point.1 The decision was made during regular monitoring of trial progress and was not part of a preplanned interim analysis. All the results reported in this article were based on deaths that occurred in participants before the date of cessation of the trial intervention.
NOTIFICATION OF DEATH DURING THE TRIAL
During the trial, participants were contacted by telephone quarterly and were asked to attend face-to-face visits annually. Examination of clinical records was performed in conjunction with these visits. In most cases, death was identified during the course of routine trial activity, when failure to establish contact led to a review of health records or when the next of kin or a close contact notified the trial center. In all cases, notification of death required confirmation from two independent sources (the family, the primary care physician, or a public death notice).
In Australia, to supplement these strategies, the trial staff performed weekly linkage with the Ryerson Index, a community-maintained register that is compiled by volunteers who monitor death notices and obituaries.14 At the end of the trial, the names of all the Australian participants, as well as the names of U.S. participants who had withdrawn or were lost to follow-up, were linked to the National Death Index in the relevant country.
ADJUDICATION OF THE UNDERLYING CAUSE OF DEATH
After a notification of death was confirmed, clinical details related to the death were sought from clinicians, hospitals, nursing homes, and hospices. The information that was compiled included autopsy reports, hospital progress notes and discharge summaries, and information obtained from the next of kin or other family members. A copy of the death certificate was requested from the relevant government agency (state-based registers of births, deaths, and marriages).
From these documents, staff at the trial coordinating center at Monash University prepared case summaries that were presented to two adjudicators, one in the United States and one in Australia. The staff members and the adjudicators were unaware of the trial-group assignments. The adjudicators examined the progression of the final illness or incident and assigned an underlying cause of death, which was considered to be the single disease that was most likely to have initiated the trajectory toward death. Discordant adjudications were resolved through consensus. In cases of death in which relevant records could not be obtained, the underlying cause of death was based on International Classification of Diseases, 10th Revision (ICD-10), codes that were recorded on the death certificate or on the results of a search of the National Death Index.
DETERMINATION OF THE PROXIMAL CAUSE OF DEATH
In addition to the underlying cause of death, the proximal cause of death was determined. Available clinical documentation was examined by clinical trial staff who were unaware of the trialgroup assignments. The proximal cause of death was considered to be the terminal event that immediately led to death (e.g., infection, bleeding, or thrombosis). In an independent assessment of cancer-related causes of death, we tabulated information from death certificates to determine whether cancer was listed as a contributing cause (Tables S4 and S5 in the Supplementary Appendix).
STATISTICAL ANALYSIS
All analyses were performed on an intention-to-treat basis. Cox proportional-hazards models were used to compare results between the aspirin group and the placebo group. Hazard ratios were calculated for death from any cause and for death related to specific causes. Analyses of subgroups that were defined according to prespecified (and some nonprespecified) baseline characteristics were performed with inclusion of interactions in the Cox models. Further details about the analyses are available in the statistical analysis plan.15 Cumulative incidences were used to show the risk of death related to each specific cause, with stratification according to trial group and with allowance for the competing risk of death from the other causes.16 Confidence intervals and P values were not adjusted for multiple comparisons.
RESULTS
PARTICIPANTS
From March 2010 through December 2014, a total of 19,114 persons (16,703 from Australia and 2411 from the United States) were enrolled in the trial, of whom 9525 were randomly assigned to receive aspirin and 9589 to receive placebo. Details regarding the characteristics of the participants have been published previously.17 Blacks and Hispanics constituted 52.7% of the 2411 trial participants from the United States. At the end of the trial, the total number of years during which participants were at risk for death (person-years) was 44,007 in the aspirin group and 44,382 in the placebo group.
ALL-CAUSE MORTALITY
A total of 1052 participants (5.5%) died during the trial. The analysis of the secondary end point of death from any cause included the 141 deaths that occurred after another primary end-point event (i.e., a diagnosis of dementia or permanent physical disability). The risk of death from any cause was 12.7 events per 1000 person-years in the aspirin group and 11.1 events per 1000 person-years in the placebo group (hazard ratio, 1.14; 95% confidence interval [CI], 1.01 to 1.29), with 1.6 excess deaths per 1000 person-years in the aspirin group. Table 1 shows the risk of death according to the major underlying causes (cancer, cardiovascular disease, and major hemorrhage), as well as the risk of death related to other causes, such as sepsis, chronic lung disease, dementia, or heart failure.
Table 1.
Mortality According to the Underlying Cause of Death.*
| Cause of Death | Overall (N = 19,114) |
Aspirin (N = 9525) |
Placebo (N = 9589) |
Hazard Ratio (95% CI) |
|---|---|---|---|---|
| no. of deaths | no. of deaths (%) | |||
| Any | 1052 | 558 (5.9) | 494 (5.2) | 1.14 (1.01–1.29) |
| Cancer† | 522 | 295 (3.1) | 227 (2.3) | 1.31 (1.10–1.56) |
| Cardiovascular disease, including ischemic stroke‡ | 203 | 91 (1.0) | 112 (1.2) | 0.82 (0.62–1.08) |
| Major hemorrhage, including hemorrhagic stroke§ | 53 | 28 (0.3) | 25 (0.3) | 1.13 (0.66–1.94) |
| Other¶ | 262 | 140 (1.5) | 122 (1.3) | 1.16 (0.91–1.48) |
| Insufficient information∥ | 12 | 4 (<0.1) | 8 (0.1) | — |
The confidence intervals shown in this table have not been adjusted for multiple comparisons, and inferences drawn from them may not be reproducible.
Data are shown for deaths that were related to primary or metastatic cancer.
Cardiovascular disease was defined as any ischemic event (myocardial infarction, other coronary heart disease, sudden cardiac death, or ischemic stroke).
Major hemorrhage was defined as any hemorrhagic event (hemorrhagic stroke, symptomatic intracranial bleeding, or major gastrointestinal bleeding or other extracranial bleeding).2
Data are shown for deaths that were related to causes that are not represented in the other categories (e.g., sepsis, chronic lung disease, dementia, or heart failure), except for deaths for which insufficient information was available to adjudicate an underlying cause.
Data are shown for deaths for which insufficient information was available to adjudicate an underlying cause, even after linkage with the National Death Index. The hazard ratio was not determined because of the low numbers of deaths.
Cancer was the underlying cause in 49.6% of the deaths, cardiovascular disease (including ischemic stroke) in 19.3%, and major hemorrhage (including hemorrhagic stroke) in 5.0% (Table 1). In only 12 cases of death (4 in the aspirin group and 8 in the placebo group), insufficient information was available to allow an underlying cause to be determined. A total of 97.6% of the deaths were detected during the trial, with 2.4% (25 deaths) identified during the final search of the National Death Index.
CANCER-RELATED MORTALITY
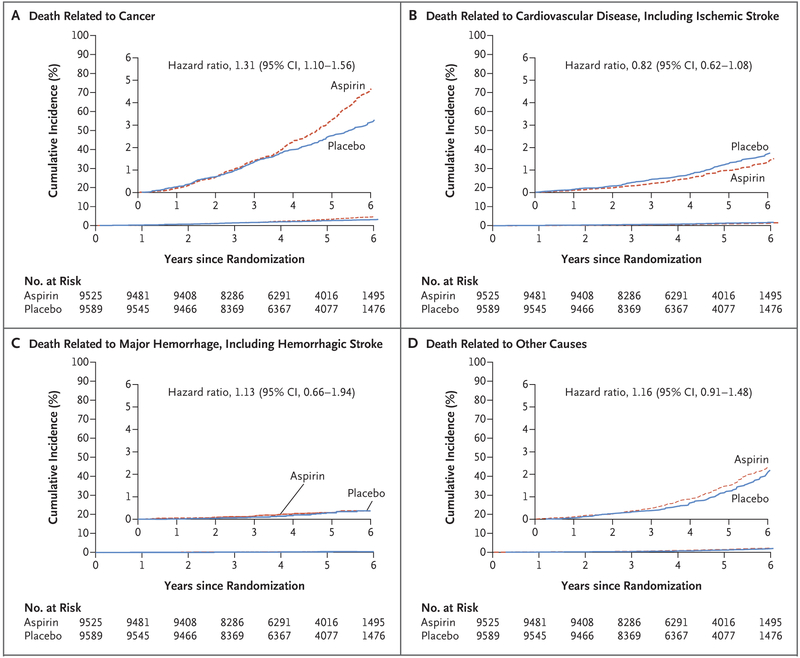
Among participants who received aspirin, the major contributor to the higher all-cause mortality was the higher risk of death for which the underlying cause was adjudicated to be cancer. The risk of cancer-related death was 6.7 events per 1000 person-years in the aspirin group and 5.1 events per 1000 person-years in the placebo group (hazard ratio, 1.31; 95% CI, 1.10 to 1.56) (Table S3 in the Supplementary Appendix). In a separate analysis that was based on a tabulation of the number of deaths in which cancer was recorded as a contributing cause on the death certificate, a similar pattern was observed, with 272 deaths (6.2 events per 1000 person-years) in the aspirin group and 206 deaths (4.6 events per 1000 person-years) in the placebo group. In curves showing the cumulative incidence of death according to each major cause, there is a progressive divergence beginning in the third year after randomization in the curves for death from any cause1 and for death related to cancer, as compared with the curves for death related to other major causes (Fig. 1).
Figure 1. Cumulative Incidence of Death According to the Underlying Cause.
Shown is the cumulative incidence of death according to major underlying causes (cancer, cardiovascular disease, and major hemorrhage) and of death related to other causes. For each cause of death, the cumulative incidence was based on a competing-risks model, which was stratified according to trial group, with the remaining causes of death as competing events. Data are not shown for 12 deaths for which insufficient information was available to adjudicate an underlying cause, even after linkage with the National Death Index. The insets show the same data on an enlarged y axis.
Table 2 shows cancer-related mortality according to the type of cancer. Despite the small number of deaths associated with each type of cancer, it is apparent that the higher cancer-related mortality in the aspirin group was not confined to specific tumor locations or pathologic types. A higher rate of death from gastrointestinal cancer (including colorectal cancer) in the aspirin group than in the placebo group contributed substantially to the overall excess mortality associated with aspirin. The excess cancer-related mortality among participants who received aspirin was seen both among those who entered the trial with a personal history of cancer (with cancer-related death occurring in 94 such participants in the aspirin group and in 88 in the placebo group) and among those in whom cancer was first diagnosed after randomization (with cancer-related death occurring in 198 and 138, respectively) (Table S3 in the Supplementary Appendix).
Table 2.
Cancer-Related Mortality According to Type of Cancer.*
| Type of Cancer | Aspirin (N = 9525) |
Placebo (N = 9589) |
Hazard Ratio (95% CI) |
||
|---|---|---|---|---|---|
|
no. of deaths |
rate per 1000 person-γr |
no. of deaths |
rate per 1000 person-γr |
||
| Any | 295 | 6.7 | 227 | 5.1 | 1.31 (1.10–1.56) |
| Lung | 55 | 1.3 | 51 | 1.2 | 1.09 (0.74–1.59) |
| Colorectal | 35 | 0.8 | 20 | 0.5 | 1.77 (1.02–3.06) |
| Pancreatic | 29 | 0.7 | 21 | 0.5 | 1.40 (0.80–2.45) |
| Hematologic | 24 | 0.6 | 19 | 0.4 | 1.27 (0.70–2.33) |
| Prostate | 18 | 0.4 | 17 | 0.4 | 1.07 (0.55–2.08) |
| Ovarian or endometrial | 15 | 0.3 | 13 | 0.3 | 1.16 (0.55–2.45) |
| Breast | 15 | 0.3 | 7 | 0.2 | 2.16 (0.88–5.31) |
| Brain | 13 | 0.3 | 9 | 0.2 | 1.46 (0.62–3.41) |
| Melanoma | 12 | 0.3 | 8 | 0.2 | 1.51 (0.62–3.70) |
| Bladder | 8 | 0.2 | 9 | 0.2 | — |
| Kidney | 9 | 0.2 | 4 | 0.1 | — |
| Gallbladder or bile duct | 7 | 0.2 | 6 | 0.1 | — |
| Stomach | 9 | 0.2 | 3 | 0.1 | — |
| Liver | 4 | 0.1 | 0 | 0 | — |
| Other | 28 | 0.6 | 27 | 0.6 | 1.05 (0.62–1.78) |
| Unknown primary | 12 | 0.3 | 7 | 0.2 | 1.73 (0.68–4.39) |
| Undetermined | 2 | 0.05 | 6 | 0.1 | — |
Some hazard ratios were not determined because of the low numbers of deaths. The confidence intervals shown in this table have not been adjusted for multiple comparisons, and inferences drawn from them may not be reproducible.
The higher cancer-related mortality among those who received aspirin was accompanied by a higher incidence of cancer among those who received aspirin, although to a lesser degree: cancer (excluding nonmelanoma skin cancer) was diagnosed in 981 participants in the aspirin group, as compared with 952 in the placebo group. Among the 66% of deaths for which information regarding the terminal phase of the illness was available, there were no apparent differences between the two trial groups in the rate of each proximal cause of death, including bleeding (Tables S4 and S5 in the Supplementary Appendix).
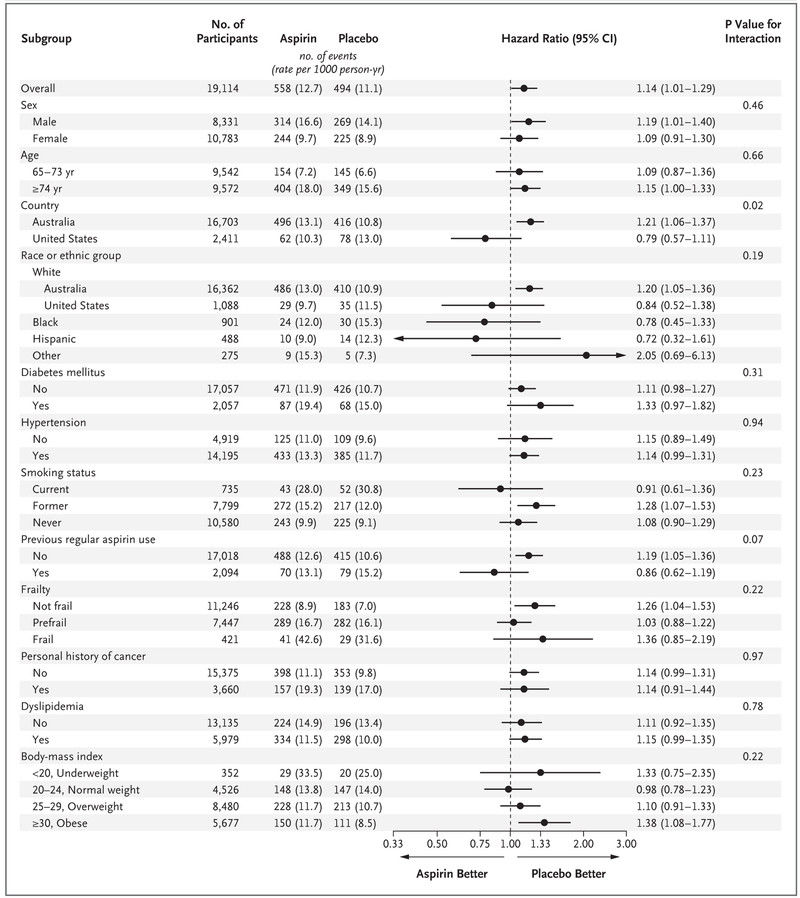
SUBGROUP ANALYSES
The effect of aspirin on all-cause mortality appeared to be consistent across a series of prespecified and nonprespecified subgroups (Fig. 2, and Fig. S1 and Table S6 in the Supplementary Appendix). The only significant interaction term was country of origin (P = 0.02); the effect of aspirin on mortality appeared to be limited to Australian participants. Interpretation of this interaction is limited because P values were not adjusted for multiple comparisons and is complicated by differences between participants from the two countries in age and race (and possibly other factors).
Figure 2 (facing page). Subgroup Analyses of All-Cause Mortality.
Race and ethnic group were reported by the participants. Other race or ethnic group was defined as any category with less than 200 participants overall, which included Aboriginal or Torres Strait Islander (12 participants), Native American (6), multiple races or ethnic groups (64), Native Hawaiian or Pacific Islander (11), and those who indicated that they were not Hispanic but did not state another race or ethnic group (18). The arrows indicate that the 95% confidence intervals were beyond the scale. The presence of diabetes was based on participants’ report of diabetes mellitus or a fasting glucose level of at least 126 mg per deciliter (≥7 mmol per liter) or receipt of treatment for diabetes. Hypertension was defined as treatment for high blood pressure or a blood pressure of more than 140/90 mm Hg at trial entry. Previous regular aspirin use was defined according to participant-reported regular use of aspirin immediately before the first baseline visit, with a 1-month washout period before randomization. Frailty was categorized on the basis of the adapted Fried frailty criteria, which included body weight, strength, exhaustion, walking speed, and physical activity.15 The category of prefrail included participants who met one or two criteria, and the category of frail included those who met three or more criteria. Dyslipidemia was defined as the receipt of cholesterol-lowering medication or as a serum cholesterol level of at least 212 mg per deciliter (≥5.5 mmol per liter) in Australia and at least 240 mg per deciliter (≥6.2 mmol per liter) in the United States or as a low-density lipoprotein level of more than 160 mg per deciliter (>4.1 mmol per liter). Body-mass index is the weight in kilograms divided by the square of the height in meters.
Figure S2 and Table S3 in the Supplementary Appendix show the difference between the aspirin group and the placebo group in cancer-related mortality according to a variety of prespecified and nonprespecified subgroups. There was no evidence of a modification in the effect of aspirin on cancer-related mortality among the examined subgroups.
In addition, Figure S3 in the Supplementary Appendix shows the hazard ratios for all-cause mortality for aspirin as compared with placebo that were reported in other major primary prevention trials involving this agent. The higher mortality in the aspirin group in this trial was an unexpected result in the context of previous trials.
MORTALITY IN THE TRIAL POPULATION AS COMPARED WITH THE GENERAL POPULATION
As a frame of reference, we examined all-cause mortality and cancer-related mortality in a simulated cohort of the general population that was matched to the trial population in age, sex, country of origin, and race or ethnic group (with data for the final characteristic available only for the U.S. participants). All-cause mortality was 34.9 events per 1000 person-years in the matched population, as compared with 11.1 events per 1000 person-years in the trial population. Cancer-related mortality was 10.5 events per 1000 person-years in the matched population, as compared with 5.1 events per 1000 person-years in the trial population.
DISCUSSION
In the randomized, placebo-controlled ASPREE trial, the use of low-dose aspirin (100 mg per day for a median of 4.7 years) did not prolong disability-free survival among elderly participants, most of whom were 70 years of age or older at trial entry.1 Death from any cause, which was a component of the primary end point (disabilityfree survival) as well as a secondary end point, occurred in 558 participants in the aspirin group (at a rate of 12.7 events per 1000 person-years) and in 494 participants in the placebo group (at a rate of 11.1 events per 1000 person-years), with a hazard ratio of 1.14. The 95% confidence interval for the hazard ratio was 1.01 to 1.29. However, the calculation of the confidence interval did not account for the fact that multiple secondary end points were analyzed. Nevertheless, the results could not rule out an increase of 1 to 29% in all-cause mortality.
The apparent higher mortality in the aspirin group than in the placebo group was explained largely by higher cancer-related mortality in the aspirin group, with mortality related to major hemorrhage contributing only minimally. Cumulative incidence curves for death from any cause1 and cancer-related death were similar in the aspirin group and the placebo group during the first 3 years of the trial. Beyond that time, the curves for these end points in the aspirin group appeared to diverge progressively from the curves in the placebo group, whereas the curves for death related to other major causes were similar in the two groups. In an exploratory analysis, the hazard ratio for cancer-related death was 1.31 (95% CI, 1.10 to 1.56).
All-cause mortality and cancer-related mortality in the trial population were 32% and 49% of the rates in the general population, respectively. The lower rates in the trial population probably reflect the healthy nature of the trial volunteers and the exclusion of participants with previous cardiovascular or cerebrovascular disease, cognitive impairment, or a physician-estimated life expectancy of less than 5 years.
In the context of multiple end points, the clinical importance of the between-group differences in death from any cause and cancer-related death is uncertain. However, the relatively large number of events, the objective nature of the end points with virtually complete ascertainment of vital status, and the progressive separation of the cumulative incidence curve for cancer-related death in the aspirin group from the curve in the placebo group are in favor of a true effect.
The higher cancer-related mortality in the aspirin group was not confined to any specific cancer location or pathologic type and was observed among both Australian and U.S. participants (Fig. S2 in the Supplementary Appendix). It could not be associated with a particular proximal cause of death, such as bleeding, which was observed rarely among the participants for whom data regarding the terminal phase of illness were available (Table S5 in the Supplementary Appendix). In fact, most participants would have stopped taking the trial intervention in advance of the terminal phase of their last illness, making it unlikely that aspirin would have contributed to higher mortality at that stage.
Primary prevention trials of low-dose aspirin that have been published previously have not shown similar higher mortality. In addition, these trials have not shown higher cancer-related mortality, although most previous studies did not include cancer as a predefined secondary end point and did not institute systematic approaches to the diagnosis and adjudication of cancer end points. These trials also differed from the ASPREE trial in their inclusion of relatively small numbers of participants 70 years of age or older. In our trial, tumor-tissue samples at diagnosis were obtained from approximately half the participants in whom cancer developed and may be useful in further exploration of the biologic mechanisms involved.18
In contrast to the ASPREE trial, meta-analyses of previous randomized prevention trials of aspirin have shown a protective effect of aspirin on cancer-related death, which became evident after 4 or 5 years of continuous therapy.19 Despite limited periods of intervention (typically ≤5 years), the preventive effect of aspirin was maintained for at least 15 years. There was also evidence of a lower risk of death from metastatic spread of cancer among participants who received aspirin than among those who received placebo.20
The biologic basis for either an early or a delayed effect of aspirin on cancer is unclear. Aspirin has been shown to influence various cellular and molecular pathways that are relevant to the initiation, progression, and spread of cancer.21 Questions may therefore arise about whether the biology of cancer differs among age groups with regard to the frequency of common molecular patterns, metastatic behavior, and treatment responses.
Strengths of the data on mortality in this trial include the size of the trial sample, particularly the large number of participants 70 years of age or older, and the access to clinical records, which allowed the underlying and proximal causes of death to be identified accurately in a high percentage of cases, despite the complex clinical scenarios that are common in this age group. The principal limitation is the limited follow-up period, which may have ended before the possible emergence of a preventive effect on cancer. The trial also focused on a specific age range and had limited statistical power on which to base firm conclusions about the effect of aspirin on mortality in subgroups of the U.S. population.
In conclusion, among healthy adults who did not have an indication for aspirin use and were predominantly 70 years of age or older at enrollment, all-cause mortality was apparently higher among those who received daily low-dose aspirin than among those who received placebo, with 1.6 excess deaths per 1000 person-years occurring in the aspirin group after a median of 4.7 years, and cancer was the principal cause of the excess deaths. Other primary prevention trials of aspirin have not identified similar results, which suggests that the mortality results reported here should be interpreted with caution.
Supplementary Material
Acknowledgments
Supported by a grant (U01AG029824) from the National Institute on Aging and the National Cancer Institute at the National Institutes of Health, by grants (334047 and 1127060) from the National Health and Medical Research Council of Australia, and by Monash University and the Victorian Cancer Agency.
Footnotes
A complete list of the ASPREE trial investigators is provided in the Supplementary Appendix, available at NEJM.org.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
A data sharing statement provided by the authors is available with the full text of this article at NEJM.org.
We thank the trial staff in Australia and the United States, the participants who volunteered for this trial, and the general practitioners and staff of the medical clinics who cared for the participants.
Contributor Information
John J. McNeil, Department of Epidemiology and Preventive Medicine, Monash University, Melbourne, Australia
Mark R. Nelson, Department of Epidemiology and Preventive Medicine, Monash University; VIC, Menzies Institute for Medical Research, University of Tasmania, Hobart, Melbourne, Australia
Robyn L. Woods, Department of Epidemiology and Preventive Medicine, Monash University, Melbourne, Australia
Jessica E. Lockery, Department of Epidemiology and Preventive Medicine, Monash University, Melbourne, Australia
Rory Wolfe, Department of Epidemiology and Preventive Medicine, Monash University, Melbourne, Australia
Christopher M. Reid, Department of Epidemiology and Preventive Medicine, Monash University; School of Public Health, Curtin University, Melbourne, Australia
Brenda Kirpach, Berman Center for Outcomes and Clinical Research, Hennepin Healthcare Research Institute, Minneapolis
Raj C. Shah, Department of Family Medicine and Rush Alzheimer’s Disease Center, Rush University Medical Center, Chicago
Diane G. Ives, Center for Aging and Population Health, Department of Epidemiology, University of Pittsburgh, Pittsburgh
Elsdon Storey, Department of Epidemiology and Preventive Medicine, Monash University, Melbourne, Australia
Joanne Ryan, Department of Epidemiology and Preventive Medicine, Monash University, Melbourne, Australia
Andrew M. Tonkin, Department of Epidemiology and Preventive Medicine, Monash University, Melbourne, Australia
Anne B. Newman, Center for Aging and Population Health, Department of Epidemiology, University of Pittsburgh, Pittsburgh
Jeff D. Williamson, Sticht Center on Aging and Alzheimer’s Prevention, Section on Gerontology and Geriatric Medicine, Department of Internal Medicine, Wake Forest School of Medicine, Winston-Salem, NC
Karen L. Margolis, Hennepin Healthcare, HealthPartners Institute, Minneapolis
Michael E. Ernst, Department of Pharmacy Practice and Science, College of Pharmacy and Department of Family Medicine, Carver College of Medicine, University of Iowa, Iowa City
Walter P. Abhayaratna, College of Medicine, Biology, and Environment, Australian National University, Canberra, ACT, Australia
Nigel Stocks, Discipline of General Practice, University of Adelaide, Adelaide, SA, Australia
Sharyn M. Fitzgerald, Department of Epidemiology and Preventive Medicine, Monash University, Melbourne, Australia
Suzanne G. Orchard, Department of Epidemiology and Preventive Medicine, Monash University, Melbourne, Australia
Ruth E. Trevaks, Department of Epidemiology and Preventive Medicine, Monash University, Melbourne, Australia
Lawrence J. Beilin, School of Medicine, Royal Perth Hospital, University of Western Australia, Perth, Australia
Geoffrey A. Donnan, Florey Institute of Neuroscience and Mental Health, University of Melbourne, Parkville, VIC, Australia
Peter Gibbs, Walter and Eliza Hall Institute of Medical Research, Australia
Colin I. Johnston, Department of Epidemiology and Preventive Medicine, Monash University; Baker Heart and Diabetes Institute, Melbourne, Australia
Barbara Radziszewska, Division of Geriatrics and Clinical Gerontology, National Institute on Aging, Bethesda, MD
Richard Grimm, Berman Center for Outcomes and Clinical Research, Hennepin Healthcare Research Institute, Minneapolis
Anne M. Murray, Berman Center for Outcomes and Clinical Research, Hennepin Healthcare Research Institute, Minneapolis; Division of Geriatrics, Department of Medicine; University of Minnesota, Minneapolis
REFERENCES
- 1.McNeil JJ, Woods RL, Nelson MR, et al. Effect of aspirin on disability-free survival in the healthy elderly. N Engl J Med 2018;379:1499–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McNeil JJ, Wolfe R, Woods RL, et al. Effect of aspirin on cardiovascular events and bleeding in the healthy elderly. N Engl J Med 2018;379:1509–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ikeda Y, Shimada K, Teramoto T, et al. Low-dose aspirin for primary prevention of cardiovascular events in Japanese patients 60 years or older with atherosclerotic risk factors: a randomized clinical trial. JAMA 2014;312:2510–20. [DOI] [PubMed] [Google Scholar]
- 4.Fowkes FGR, Price JF, Stewart MCW, et al. Aspirin for prevention of cardiovascular events in a general population screened for a low ankle brachial index: a randomized controlled trial. JAMA 2010;303:841–8. [DOI] [PubMed] [Google Scholar]
- 5.Ogawa H, Nakayama M, Morimoto T, et al. Low-dose aspirin for primary prevention of atherosclerotic events in patients with type 2 diabetes: a randomized controlled trial. JAMA 2008;300:2134–41. [DOI] [PubMed] [Google Scholar]
- 6.Belch J, MacCuish A, Campbell I, et al. The Prevention of Progression of Arterial Disease and Diabetes (POPADAD) trial: factorial randomised placebo controlled trial of aspirin and antioxidants in patients with diabetes and asymptomatic peripheral arterial disease. BMJ 2008;337:a1840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ridker PM, Cook NR, Lee I-M, et al. A randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in women. N Engl J Med 2005;352:1293–304. [DOI] [PubMed] [Google Scholar]
- 8.de Gaetano G Low-dose aspirin and vitamin E in people at cardiovascular risk: a randomised trial in general practice. Lancet 2001;357:89–95. [DOI] [PubMed] [Google Scholar]
- 9.Hansson L, Zanchetti A, Carruthers SG, et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. Lancet 1998;351:1755–62. [DOI] [PubMed] [Google Scholar]
- 10.The Medical Research Council’s General Practice Research Framework. Thrombosis prevention trial: randomised trial of low-intensity oral anticoagulation with warfarin and low-dose aspirin in the primary prevention of ischaemic heart disease in men at increased risk. Lancet 1998;351:233–41. [PubMed] [Google Scholar]
- 11.Steering Committee of the Physicians’ Health Study Research Group. Final report on the aspirin component of the on-going Physicians’ Health Study. N Engl J Med 1989;321:129–35. [DOI] [PubMed] [Google Scholar]
- 12.Peto R, Gray R, Collins R, et al. Randomised trial of prophylactic daily aspirin in British male doctors. Br Med J (Clin Res Ed) 1988;296:313–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.ASPREE Investigator Group. Study design of ASPirin in Reducing Events in the Elderly (ASPREE): a randomized, controlled trial. Contemp Clin Trials 2013;36:555–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.The Ryerson Index home page (https://www.ryersonindex.org/).
- 15.Wolfe R, Murray AM, Woods RL, et al. The ASPirin in Reducing Events in the Elderly trial: statistical analysis plan. Int J Stroke 2018;13:335–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Andersen PK, Geskus RB, de Witte T, Putter H. Competing risks in epidemiology: possibilities and pitfalls. Int J Epidemiol 2012;41:861–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McNeil JJ, Woods RL, Nelson MR, et al. Baseline characteristics of participants in the ASPREE (ASPirin in Reducing Events in the Elderly) study. J Gerontol A Biol Sci Med Sci 2017;72:1586–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chan AT, Ogino S, Fuchs CS. Aspirin and the risk of colorectal cancer in relation to the expression of COX-2. N Engl J Med 2007;356:2131–42. [DOI] [PubMed] [Google Scholar]
- 19.Rothwell PM, Fowkes FGR, Belch JFF, Ogawa H, Warlow CP, Meade TW. Effect of daily aspirin on long-term risk of death due to cancer: analysis of individual patient data from randomised trials. Lancet 2011;377:31–41. [DOI] [PubMed] [Google Scholar]
- 20.Rothwell PM, Wilson M, Price JF, Belch JFF, Meade TW, Mehta Z. Effect of daily aspirin on risk of cancer metastasis: a study of incident cancers during randomised controlled trials. Lancet 2012;379:1591–601. [DOI] [PubMed] [Google Scholar]
- 21.Drew DA, Cao Y, Chan AT. Aspirin and colorectal cancer: the promise of precision chemoprevention. Nat Rev Cancer 2016;16:173–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.